Commentary by Bill Sardi
via Orthomolecular Medicine News Service
(OMNS Aug 31 2018) Here we go again. Another physician says there "no case for vitamin supplementation in normal, healthy, non-pregnant or lactating adults who are receiving the recommended daily intake of nutrients." [1]
Here is my comment on each of the criticisms about dietary supplementation.
Vitamin A
Vitamin critic: "Vitamin A Toxicity occurred in Antarctic and Arctic explorers who consumed the livers of seals, huskies or polar bears and can be fatal. It is characterized by raised intracranial pressure, dermatitis, nausea and vomiting, double vision and convulsions.
Rebuttal: Yes, we are talking about millions of units of vitamin A. Let's concede this point. All consumers who are eating seal or polar bear liver should refrain from doing so.
Vitamin critic: Of particular concern are other data that have linked vitamin A to an 18% increased incidence of lung cancer in a study of 29,133 Finnish smokers who received either alpha-tocopherol (vitamin E) 50 mg or beta-carotene 20 mg and a 28% increase of lung cancer in a similar study in 18,314 smokers, some of whom had also been exposed to asbestos.
Rebuttal: Not this one again? This study was published in the New England Journal of Medicine just prior to passage of the 1994 Dietary Supplement Health & Education Act in an attempt to legislatively classify all dietary supplements as drugs.[2] Here (below) a chart from that study reveals the quoted 18% difference in lung cancer incidence was only a relative number, but in absolute numbers the difference was very small, less than 1%.
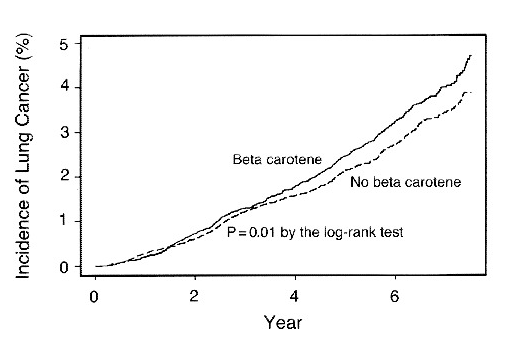
Source : New England Journal Medicine [2]
And 18 years after this study was published it was revealed that excessive vitamin A supplementation via beta carotene (which converts to vitamin A in the body) impairs vitamin D blood levels and negates any reduction in lung cancer achieved by vitamin D supplementation. Vitamin D supplements were found to reduce the risk of lung cancer in sun-deprived Finnish men, but not when they consumed excessive amount of vitamin A.[3] These Finnish men needed more vitamins, not less.
Excessive beta carotene is shuttled to the skin to provide internal sun protection and is not toxic to the liver as is mega-dose vitamin A. Most reports of liver toxicity from vitamin A supplementation emanate from alcoholics whose livers are compromised by their drinking habit.
The Council For Responsible Nutrition (CRN) says: "the human data, however, are often confounded by other factors such as alcohol intake, infectious hepatitis, hepatotoxic drugs, and pre-existing liver disease."
According to a CRN report: Consumption of 25,000 to 50,000 IU of preformed vitamin A per day for periods of several months or more can produce multiple adverse effects, including liver toxicity; but the effects in this intake range may be dependent on compromised liver health or function.[4] A supplemental intake of approximately 25,000 IU is the lowest dose at which such effect can be confidently attributed to vitamin A in persons with mildly or moderately compromised liver health.
Vitamin critic: The vitamin critic (whose name shall remain unmentioned) warns consumers away from vitamin A supplements, saying: "the Upper Limit for both sexes is 10,000 IU per day."
Rebuttal: However, the Upper Limit (UL) is the perfectly safe upper limit, not the toxic limit. The Institute of Medicine states "the No Observed Adverse Effects Level (NOAEL) of intake is 15,000 international units (IU) of vitamin A per day." There is a long history of safe use of dietary supplements containing 5,000, 8,000, and 10,000 IU per day," says a CRN report.
Vitamin critic: "Particular care is needed not to exceed recommended doses (of vitamin A) in pregnancy because of the possibility of miscarriage and birth defects."
Rebuttal: The CRN states: a dose of 30,000 IU per day "should be considered as non-teratogenic (doesn't cause birth defects) in [humans]. [4]"
Vitamin D
Vitamin critic: At present there is no case for routine supplementation of vitamin D unless there is a clinical or biochemical indication. The Upper Limit for both sexes is 80 micrograms/day (320 IU - international units).
320 IU (international units) won't even raise blood levels. Thirty minutes of total body midday summer sunshine (11 AM - 2 PM) will produce ~10,000 units of vitamin D without side effects. Those with dark skin may need 4-fold longer exposure times. In winter, when the sun rises no more than 45 degrees above the horizon in the US, Canada, and Europe, the midday sun provides no more than 5% of the UVB rays that generate vitamin D compared to exposure to midday sunlight in the summer.
This recommendation is in the face of an epidemic of sun-deprivation disorders. A study recently showed children are only getting 7 hours of outdoor sunshine per week. [5] Those who work inside, for example, office workers commonly are deficient throughout the year. Further, sunblock absorbs the UVB rays and causes deprivation of vitamin D from sunlight.
An Institute of Medicine report indicates about one-quarter of the US population are at risk of vitamin D inadequacy and 8% are at risk of vitamin D deficiency (2001-06). [6] This amounts to millions of people. Supplements of vitamin D are therefore necessary.
Vitamin C
Vitamin critic: High doses are definitely associated with adverse reactions so there does not seem to be any place for routine supplementation in healthy individuals. RDI for both sexes is 45 mg/day without an UL.
Rebuttal: Vitamin C is depleted by illness and stress, and readily gets oxidized doing its antioxidant function. The body can regenerate vitamin C to some extent in red blood cells.[7] But this regeneration function is easily overwhelmed in sickness and even by everyday physical and mental stress. A few milligrams of vitamin C (~110 mgs per day) obtained from the diet cannot compensate for a gene mutation that occurred long ago in human history that halted the internal production of vitamin C. Prior to that gene mutation it is estimated that early primates, (our distant ancestors) endogenously produced 1800-4000 milligrams of vitamin C per day, and more when under physical or mental stress.[8] After major surgery, when vitamin C levels can go to zero, 3,000 mg of IV vitamin C has been found necessary to bring the level back to normal. [9] A similar depletion can occur under ordinary stress or in common viral illnesses. This is the rationale for supplementing with high doses of vitamin C. The equivalent dose to 3,000 mg IV is 10,000-20,000 mg in divided oral doses.
The vitamin critic's disclaimer is "There is no case for vitamin supplementation in normal, healthy, non-pregnant or lactating adults who are receiving the recommended daily intake of nutrients." But how many are truly healthy?
Diabetics have a higher need for vitamin C (100 million). Aspirin users (~50 million), users of certain drugs (steroids, sex hormones), smokers (38 million), alcohol abusers (16 million), face depletion of vitamin C. Diuretics deplete vitamin C (~20 million) Growing children need more vitamin C. Hospitalized patients and nursing home patients need more vitamin C. That amounts to over 200 million Americans out of a population of 325 million who are not likely to have adequate vitamin C intake from their diet and must rely upon dietary supplements.
Vitamin critic: The vitamin critic says the Recommended Dietary Allowance (RDI) both sexes is 45 mg/day of vitamin C without an Upper Limit. Public health authorities recommend 60-200 milligrams of supplemental vitamin C to maintain health.
Rebuttal: The perfectly safe Upper Limit is 2000 milligrams is often mis-characterized as the toxic upper limit. Makers of vitamin C pills seem to know better and the lowest dose vitamin C pill on the market today contains 500 milligrams. Vitamin C is water-soluble and so is readily excreted, but when its level is depleted, e.g. during stress or illness, divided doses of up to 20,000 mg/d or more do not cause gastrointestinal upset and may be required to allow the body to quickly recover.
Thiamine (vitamin B1)
Vitamin critic: The vitamin critic says there are no indications for routine supplementation of vitamin B1.
Rebuttal: Derrick Lonsdale MD says high carbohydrate diets, sugary foods, block vitamin B1 absorption, a problem he calls "high calorie malnutrition." Alcohol, coffee, tea, also block B1 absorption. The vitamin critic warns of side effects from high doses, but absorption is dose limited to 5 mg per day. The body won't absorb any more.
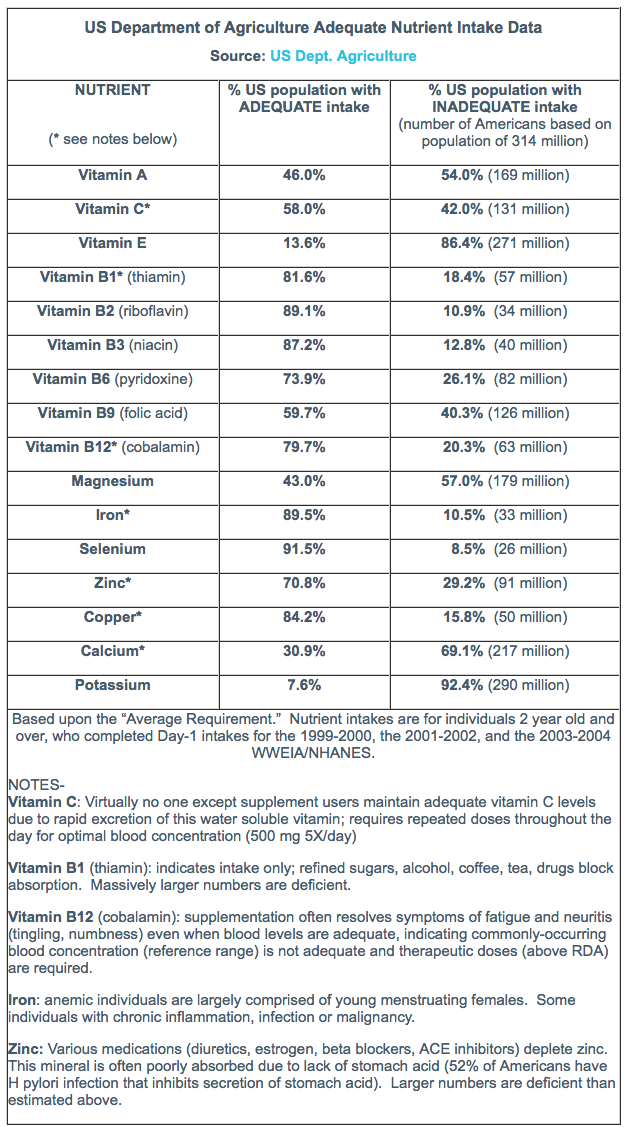
Summary: The US Department of Agriculture publishes the percent of the US population with inadequate intake of essential nutrients. It is worth reprinting here:[10]
Summary
Many people are deficient in vitamins and minerals. The vitamins discussed here, vitamins A, B1, C, and D, are commonly deficient in up to 50% of the US population (millions of people), even by the meager standards of the US Department of Agriculture. For optimum health most people should be eating a diet that includes raw vegetables and nuts, moderate amounts of meat and fish, lots of green leafy vegetables, and a variety of colored vegetables and fruits, as well as supplements with adequate doses of the B vitamins (B1-B6, B12, folate, biotin), as well as vitamins C, D, and E.
References:
1. Kennedy M. (2018) The vitamin epidemic: what is the evidence for harm or value? Intern Med J 48:901-907. https://onlinelibrary.wiley.com/doi/full/10.1111/imj.13976
2. Alpha-Tocopherol, Beta Carotene Cancer Prevention Study Group. (1994) The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N Engl J Med. 1994 Apr 14;330(15):1029-35. https://www.ncbi.nlm.nih.gov/pubmed/8127329
3. Cheng TY, Neuhouser ML. (2012) Serum 25-hydroxyvitamin D, vitamin A, and lung cancer mortality in the US population: a potential nutrient-nutrient interaction. Cancer Causes Control. 2012, 23:1557-1565. https://www.ncbi.nlm.nih.gov/pubmed/22829430
4. Vitamin A (2013). Vitamin and Mineral Safety 3rd Edition (2013) Council for Responsible Nutrition (CRN) www.crnusa.org. https://www.crnusa.org/sites/default/files/files/resources/05-CRNVMS3-VITAMINA.pdf
6. Looker AC, Johnson CL, Lacher DA, et al., (2011) Vitamin D Status: United States, 2001-2006. NCHS Data Brief U.S. Dept of HHS, CDC, National Center for Health Statistics No. 59 March 2011. https://www.cdc.gov/nchs/data/databriefs/db59.pdf
7. Montel-Hagen, A, Sitbon M, Taylor N. (2009) Erythroid Glucose Transporters. Curr Opin Hematol 16:165-172. https://www.ncbi.nlm.nih.gov/pubmed/19346941
8. Stone I. (1966) Hypoascorbemia, the genetic disease causing the human requirement for exogenous ascorbic acid. Perspect Biol Med. 1966. 10:133-134. https://muse.jhu.edu/article/406386/pdf
9. Berger MM. (2009) Vitamin C Requirements in Parenteral Nutrition. Gastroenterology 137:S70-S78. https://www.ncbi.nlm.nih.gov/pubmed/19874953
SUBSCRIBE TO OMNS: http://orthomolecular.org/subscribe.html
OMNS ARCHIVES: http://orthomolecular.org/resources/omns/index.shtml
